Princeton
Docket # 10-2608
Researchers in the Department of Chemical and
Biological Engineering, Princeton University and in the Department of
Pharmaceutics, Rutgers University have developed a targeted lung-specific
delivery system which employs both passive and active targeting to intravenously
deliver anti-cancer drugs to tumor cells as well as to reduce the occurrence of
metastasis. The first layer of the delivery system is a gel microparticle (GMP)
designed to take advantage of the venous lung filtration pathway and passively
accumulate in the lungs after intravenous injection into the body. The second
layer of the delivery system consists of two types of nanoparticles (NP)
embedded in the GMP. The NP surfaces are decorated with ligands to actively
target cancer cells. The first type of NP will be loaded with an anti-cancer
drug, while the other type of NP will be designed to irreversibly bind to cancer
cell surface receptors to inhibit metastasis. The release rate of the NPs from
the GMPs into the tumor and the release rate of the anti-cancer drug from the
NPs can be tuned to achieve the maximum desired effect. This dual-delivery
system affords the ability to sustain a high concentration of anti-cancer drugs
in the lungs while minimizing the systemic exposure and accordingly reducing the
side effects. Additionally, it may actively prevent the spread of the cancer to
other parts of the body.
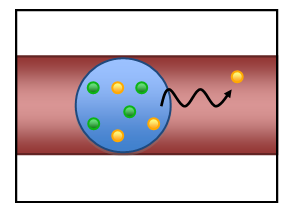
Figure 1. Embedded with drug loaded
nanoparticles (yellow) and metastasis inhibiting nanoparticles (green), the gel
microparticle (blue) is trapped in a lung capillary (red). The nanoparticles are
released overtime in the lung to kill cancer cells and prevent
metastasis.
Advantages
·
Unique
targeting options to the lungs
·
Control
of metastasis
·
Use
of alternative delivery via the venous blood stream
·
Achievement
of effective lung concentrations, while minimizing systemic exposure and
toxicity
·
Adaptable
to incorporate novel anti-cancer, TB, and COPD drugs
Commercial
Applications
This dual GMP-NP delivery system has potential
commercial application for treatment of Non-Small Cell Lung Cancer (NSCLC). The
delivery system is versatile and can be easily adapted to incorporate novel,
anti-cancer drugs as they are developed. This allows for the system to evolve
with the molecular advances in medicine and remain a relevant treatment option
for years to come. The biocompatibility and safety of the gel used have been
tested and approved by the FDA, which minimizes the regulatory delay in
implementing this new technology. The drug we propose to deliver, Camptothecin
is a current standard of care and is FDA approved.
This technology could also be developed to treat other
diseases of the lung such as asthma, tuberculosis and chronic obstructive
pulmonary disease (COPD).
Stage
of Development
Following a recent award from the NIH, a three year
timeline to develop and test the effectiveness of the dual drug delivery system
is proposed. The first step in creating the drug delivery system is to
synthesize NP loaded GMPs that accumulate in the lung with minimal toxicity. To
this end, the Sinko group at Rutgers has bounded the required size of GMPs to
passively accumulate in rat lungs between 6 and 30 μm depending on the
deformability of the particles. Current work is focused on using microfluidics
to controllably create GMPs of the appropriate size and NP loading. Degradation
of GMPs and subsequent release of NP is also being investigated. Once a suitable
delivery system has been engineered, mouse studies will be undertaken to assess
the toxicity and effects of GMPS on lung function.
The
second step is to create the cancer targeting NPs and test the dual drug
delivery system. The Prud¿homme group at Princeton has expertise in creating
nearly mono-dispersed NPs loaded with hydrophobic drugs using Flash
Nanoprecipitation (FNP). Additionally, the Prud¿homme group has previously
created NPs via FNP with cancer targeting ligands on the surface. To create the
drug loaded NPs, Camptothecin (CPT) will be incorporated into the NPs. CPT was
chosen based on previous group experience with the drug. Two active targeting
approaches that can be incorporated into NPs have been identified as possible
routes to inhibit cancer metastasis. The first is to functionalize the NP
surface with a ligand that will bind to specific cell receptors and prevent the
pro-metastatic signaling pathway. The other is to load the NPs with chemical
agents known to inhibit pro-metastatic signaling. Both cell and mice studies
will be conducted to assess the efficacy of the drug delivery system to kill
cancer cells and disrupt the pro-metastatic signaling pathway.
Background
The American Cancer Society estimated that in 2009,
1,479,350 new cancer cases would be diagnosed in the United States of which
219,440 would be lung and bronchus related. Although only the second most
prevalent type of cancer, behind prostate and breast cancer for men and women
respectively, lung cancer is the most lethal accounting for a projected 159,390
deaths in the United States. Non-small cell lung cancer (NSCLC), a subset of
lung cancer, encompasses a set of diseases with similar prognosis and
treatments. The standard treatments for NSCLC include surgery, chemotherapy,
radiation, laser and photodynamic therapy, all with various success rates
depending on the stage of the cancer. National Cancer Institute assesses,
however, that results of standard treatment are generally poor with only a 15
percent 5-year survival rate for combined cancer stages. Challenges facing the
current chemotherapy drugs include excessive toxicity to healthy tissues and
limited ability to prevent metastases. The dual drug delivery system described
herein aims to overcome these two challenges by selectively targeting the lung
to deliver anti-cancer drugs and inhibit the formation of metastases.
The design of the human lung affords unique targeting
options. Delivery via inhalation of anti-cancer drugs has been explored;
however, low absorption and poor lung distribution of drugs has limited this
avenue. A more promising approach involves passive targeting of the lung via the
venous blood stream. The lung receives the entire venous blood supply from the
heart and passes it through the intricate capillary beds on the alveoli. Large
particles in the venous blood are thus trapped in these capillary beds. This
filtering phenomenon can be used to selectively deliver particles to the lung.
Such delivery methods have been safely employed in pulmonary perfusion
diagnostic agents; however the use of this novel delivery route for
chemotherapeutic drugs has not been appreciated or utilized by the drug delivery
community. Initial IP for this mode of delivery has been filed by our
collaborator, Dr. Patrick Sinko of Rutgers University, and additional IP on the
production of nanoparticles and combination of the gel particles and specific
drug formulations have been filed.
Principal Inventors
Robert K Prud¿homme
Professor Prud¿homme is Professor of Chemical and
Biological Engineering, Department of Chemical and Biological Engineering and
the Director, Program in Engineering Biology, at Princeton University.
His research focuses on how weak forces at the molecular level determine
macroscopic properties at larger length scales. Equal time is spent on
understanding the details of molecular-level interactions using NMR, neutron
scattering, x-ray scattering, or electron microscopy and making measurements of
bulk properties such as rheology, diffusion of proteins in gels, drop sizes of
sprays, or pressure drop measurements in porous media. The work is highly
interdisciplinary; many of the projects involve joint advisors and
collaborations with researchers at NIH, Argonne National Labs, CNRS in France,
or major corporate research.
Professor Patrick Sinko
Professor Sinko is Associate Vice President for Research and Professor II
(Pharmaceutics), and holds
the Parke-Davis Endowed Chair in Pharmaceutics and Drug Delivery at Rutgers
University. Dr. Sinko's research is focused on the mechanisms and applications
of biopharmaceutics and polymers to drug delivery and targeting. Professor
Sinko¿s research efforts focus on the design, fabrication and evaluation
of molecular-scale drug and diagnostic delivery technologies applied broadly to
asthma, AIDS, cancer, and chemical counterterrorism.
Professor Howard Stone
Professor Stone is the Donald R. Dixon and Elizabeth W. Dixon
Professor of Mechanical and Aerospace Engineering at Princeton University. His
research interests lie in the broad space of the dynamics of complex fluids,
which encompass multiphase flows, colloid science, physical chemistry,
biophysics, and physicochemical hydrodynamics. Using experiments, simulations,
and modeling the objective is to quantitatively characterize problems and to
explore new research directions. Whenever possible, we actively collaborate with
industry and scientists and engineers from many disciplines. For example, these
collaborations involve home and personal care products, oil-field services,
fiber coating, float-glass manufacturing, and medical/clinical
applications.
Intellectual Property and status:
Patent pending
Contact
Laurie Tzodikov
Princeton University Office of Technology Licensing ¿ (609) 258-7256¿
tzodikov@princeton.edu
PU #10-2620